Choosing the right foods
Your diet will vary based off of your general needs, but will be most impacted by your stage of kidney failure and if end-stage renal disease, what type of dialysis treatment you are receiving.
An example from the recommended diet chart is the amount of protein recommended for pre-dialysis and for dialysis patients.
Protein
Studies have shown that a low protein diets (hypoproteic) can help postpone dialysis. (1)
Protein is important in your diet because it helps keep the body nourished and healthy to fight off potential infections, repair tissue and for growth. Quality sources of protein include lean red meat, chicken, turkey, fish, lean pork, dairy and egg products. To keep a healthy diet overall it is best to select trimmed cuts of meat or low fat dairy. Nuts and beans are also a good source of protein, but also contain phosphorus.
The chart below was derived from data in the United States Department of Agriculture (USDA) National Nutrient Database for Standard Reference, Release 20.
|
Type of Protein Source |
Amount of Protein in Grams2 |
|
Poultry |
|
|
Chicken Breast (1/2 piece) |
26 |
|
Turkey (3oz) |
24 |
|
Ground Turkey (1patty) |
22 |
|
Beef |
|
|
Top Round (3oz) |
31 |
|
Veal (3oz) |
30 |
|
Ground Beef |
22 |
|
Pork |
|
|
Pork Chop (3oz) |
25 |
|
Pork Shoulder (3oz) |
27 |
|
Ham (3oz) |
18 |
|
Seafood |
|
|
Lobster (3oz) |
17 |
|
Crab (3oz) |
16 |
|
Shrimp (6large) |
10 |
|
Fish |
|
|
Fresh Tuna (3oz) |
25 |
|
Canned Tuna (3oz) |
21 |
|
Salmon |
23 |
|
Eggs |
|
|
Egg substitute (1/4 cup) |
7 |
|
Egg Cooked (1egg) |
6 |
|
Egg White (1egg) |
3 |
|
|
|
|
Beans and Nuts |
|
|
Kidney beans (1 cup) |
15 |
|
Lima beans (1 cup) |
15 |
|
Mixed nuts (3oz) |
15 |
Calcium
Calcium is another important element in a kidney friendly diet. Healthy kidneys help balance the amount of calcium and phosphorous in the body to promote bone growth and maintenance. Too much calcium can lead to harmful hardening of vessels and too little leads to weak bones. In many dialysis patients phosphorus levels will be higher and additional calcium might be needed to restore the balance. Calcium is found in most dairy products, but these also normally contain high levels of phosphorus. Calcium supplements are an option and sometimes calcium based phosphate binders are prescribed to increase calcium and lower phosphorous levels. If calcium levels are too high there are also options. Calcimimetics can be prescribed that mimic the action of calcium and lower the amount of calcium in your body.
Your dietician will also be able to point out foods that are high in calcium. (please note many items on this list contain high levels of phosphorus)
- Dairy such as Milk, Cheeses, Yogurt and ice cream
- Spinach
- Broccoli
- Rhubarb
- Tofu
- Oranges
- Flax seeds
- Quinoa
- Nuts
- Now many common foods have added calcium (calcium fortification or enrichment) including
- Breakfast cereals and bars
- Breads
- Juices
- Margarines
- Sports drinks
- Pancake or biscuit batter
- Crackers
- Soy or rice milk
- A few foods contain calcium and low phosphorous
- Two teaspoons of cinnamon has 50mg of calcium and no phosphorous
- Two teaspoons of basil have 63mg of calcium and only 15mg of phosphorous. (2)
Potassium
Potassium is also important in your diet because potassium levels control nerve and muscle functions. Since healthy kidneys remove excess potassium, most pre-dialysis and dialysis patients have too much potassium in their diet. Potassium intake is less of an issue for PD patients and more than three times weekly, hemodialysis patients, due to the more constant cycling of fluid.
Hyperkalemia or high levels of potassium in the body is associated with a significant increase in an irregular heartbeat and sudden death. (3)
It is difficult to limit potassium in your diet, since most foods have at least some in them.
A few helpful steps to keep your level lower includes:
- Watching portion sizes of fruits and vegetables
- Rinsing canned fruits and vegetables
- Replace dairy products with non-dairy substitutes
- Avoid salt substitutes
- Try leaching (a soaking process before cooking) your vegetables
- Track your potassium levels and share any drastic changes with your dietician
|
Category |
Eat this |
Not that |
|
Fruits |
Apple |
Bananas |
|
|
Plum |
Oranges |
|
|
Berry |
Raisins |
|
Vegetables |
Zucchini |
Acorn/Butternut Squash |
|
|
Bell pepper |
Tomato |
|
|
Green bean |
Spinach |
|
Dairy |
Nondairy creamer |
Milk |
|
|
Sherbet/popsicle |
Ice Cream |
|
|
Cream Cheese |
Cheese |
|
Snacks |
Pretzels |
Nuts or Seeds |
|
|
Lemon flavored deserts |
Chocolate flavored |
|
|
Sugar cookies |
Molasses cookies |
|
|
|
|
Sodium
Sodium is one your bodies’ major electrolytes that helps control the fluid content of your tissues and cells. Most people know sodium as salt, but salt is a compound made up of sodium and chloride. Healthy kidneys remove excess sodium from the body. Too much sodium is an issue because fluid will build up leading to higher blood pressure and potentially heart failure. Sodium will also make you feel thirstier and make it more difficult to keep within your recommended fluid restrictions. PD patients don’t need to watch their sodium intake as closely as HD patients, but still need to limit their sodium intake for their overall health. Many foods that you eat have sodium, and of course some are better than others.
High levels of sodium can lead to:
- Swelling (edema) throughout your body
- High blood pressure (hypertension)
- Heart failure
- Shortness of breath
Low sodium choices include:
- Fresh fruits and vegetables
- Unsalted popcorn
- Breads
- Pastas
- Unprocessed meats
High sodium choices to avoid include:
- Processed meats such as ham and luncheon meats
- Chips
- Canned soups and vegetables
- Tomato juice
- Sports drinks
- Many fast or convenience foods
You can help manage your intake by:
- Keeping a food journal to track your dietary sodium.
- Recording your weight daily to track swelling.
- Limiting processed foods.
- Choosing low sodium alternatives and not adding additional salt to meals.
- Reading food labels and looking for hidden sodium in items like drinks or in canned goods.
- Using natural flavor enhancers like spices and herbs as a substitute for salt.
What about dining out?
Restaurants don’t have to be off-limits. You can stick with a kidney-friendly diet and still enjoy your favorite places to eat. Work with your renal dietitian and learn to plan ahead. He or she will be able to give you suggestions based off of the type of food you are going for. Also if you know you are going for a specific type of food you can limit that type of food in your other meals that day. For example if you are going out for Mexican and really want salsa then you can try to limit your potassium in the other items that you eat.
Remember restaurant portions are often larger than those you eat at home. You can always ask for half to be boxed up in the beginning or share a meal with your table.
Don’t be afraid to ask your server for special requests, such as sauce on the side or no salt. The worst thing they can do is say no. Also, remember to bring your phosphate binders with you and take them as directed with your meal.
Don’t get caught up on what you can’t have, but use this as an opportunity to try something new and enjoy!
|
INSTEAD OF |
TRY |
|
Mexican |
|
|
tomato-based salsa |
chili pepper salsa |
|
avocado, mango, papaya, guava |
fajitas where you can control the condiments you add |
|
beans, Spanish rice |
plain rice |
|
Italian |
|
|
tomato and cream sauces |
pesto sauce |
|
olives and cheeses |
Breaded calamari |
|
pizza with pepperoni, sausage, olives, anchovies |
(white pizza)pizza with chicken and peppers |
|
cheese ravioli with tomato sauce |
Grilled fish, veal picatta, shrimp scampi |
|
Asian |
|
|
extra soy sauce, fish sauce and MSG (monosodium glutamate) |
ginger, hot pepper oil |
|
fried rice |
steamed rice |
|
meat, fish and/or poultry mixed with sauce |
grilled fish and chicken, tempura, sushi (no California rolls with avocado) or stir-fried vegetables with sauce on the side |
|
Southern |
|
|
dried beans or black eyed peas |
string beans or corn |
|
salted/cured meats, sausages, bacon, salt pork |
fried chicken with the skin removed |
|
cooked greens or spinach |
Okra |
|
Fast Food |
|
|
milkshake |
small ginger ale or lemon-lime soda |
|
French fries, baked potato |
Rice |
|
large, super- or king-sized hamburgers or cheeseburgers |
regular or junior-sized hamburgers |
How to read food labels
Food labels are a great tool. They can help you choose healthier, more kidney-friendly foods. However, before you go to the grocery store, talk with your renal dietitian. Since you need to watch certain nutrients such as potassium and phosphorous that were highlighted earlier in this course. Your renal dietitian can tell you how many milligrams (mg) or how much you should have each day. Once you know this, you’re ready to shop. (4)
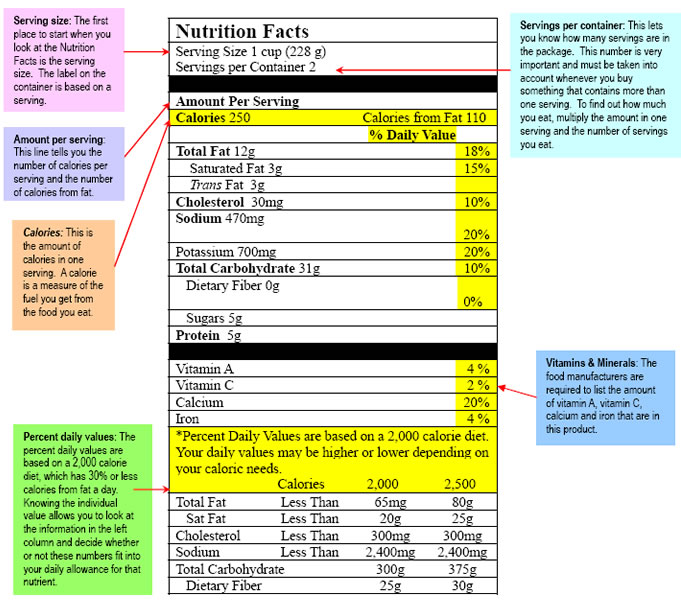
Food label tips:
- Items that you need to look out for are generally listed by content in grams or milligrams and percent daily values. It is important to remember that these values are for someone without kidney disease, so your needs may differ.
- A good rule of thumb is: food is low in phosphorus if it has fewer than 50 mg (or less than 5%). It’s high in phosphorus if it has more than 150 mg (or greater than 15%). (5)
- In general, a food is low in potassium if it has fewer than 100 mg (or less than 3%). More than 200 mg (or greater than 6%) is high. (6)
- Be aware. If a food label doesn’t list an item such as phosphorus in the example image, it doesn’t mean it isn’t in there.
- Another important thing to look at is serving size. For example a 20oz bottle of cola has 2.5 servings per bottle. If you drank the entire bottle, the values would need to be multiplied by 2.5.
- When in doubt, you can always save the labels and go over questions with your dietician.
Modify your favorite recipes
Cooking at home is a great way to save money and also put you in control of what you are eating. Living on a kidney friendly diet does mean that you have to limit or modify your recipes, but doesn’t mean you can’t enjoy meals with your family. In fact, sharing meals can be a good way to come together.
Keeping a journal and meal planning will help you stay on your diet and buying foods in bulk that can be used for multiple meals will keep your shopping costs down.
Family meals should be a source of comfort and not stress. Your family loves and cares for you so they will be willing to compromise. Getting everyone involved will help make those decisions easier.
There are many resources for dialysis friendly recipes here are some compiled by DaVita that can be used as a starting point.
Also, your dietician and other members of your care team will be able to point you towards flavorful foods.
Just like dining out, this will give you a chance to try new items and expand your choices. Maybe you and your family will discover a new appreciation for pesto sauces instead of tomato based.
- Capusa C, Garneata L, Mircescu G, Stancu, S. Effects of a Supplemented Hypoproteic Diet in Chronic Kidney Disease. Journal of Renal Nutrition Volume 17, Issue 3 May 2007.
- USDA National Nutrient Database for Standard Reference, Release20. National Agriculture Library. http://www.nal.usda.gov/fnic/foodcomp/Data/SR20/nutrlist/sr20a203.pdf
- Sudden Cardiac Death in Hemodialysis Patients: An In-Depth Review. American Journal of Kidney Disease. http://www.ajkd.org/article/S0272-6386(11)00595-6/fulltext#sec2.4
- Reading Nutritional Labels on Food Labels. Children’s Hospital of The King’s Daughters. http://www.chkd.org/HealthLibrary/Facts/Content.aspx?pageid=0416
- Phosphorus and your CKD Diet. National Kidney Foundation. www.kidney.org/atoz/content/phosphorus.cfm
- Potassium and you CKD Diet. National Kidney Foundation. http://www.kidney.org/atoz/content/potassium.cfm